Telemedicine set for steady rise after pandemic: Experts

Telemedicine, cited in a recent survey as having had the largest impact on workers compensation during the COVID-19 pandemic, appears poised to keep growing even as states reopen, experts say.
9 Ways Virtual Reality (VR) Is Improving Healthcare Right Now

Technology and medicine go hand in hand. Check out how VR is making healthcare better for everyone right now.
Best Exercises for Diabetes & Pre-Diabetes

If you have diabetes or pre-diabetes, you’ve probably heard from your physician about the importance of a good diet and regular exercise. Consistent body movement (which goes beyond walking to the fridge) will help boost energy, better manage blood sugar levels, reduce insulin needs, manage stress, improve your mood and promote better sleep. If you’re […]
6 Companies That Are Taking Telemedicine By Storm

As with much of our “new normal,” consumers’ newfound telehealth habit won’t be going anywhere. Demand for telemedicine is expected to rise by 38% over the next five years as more and more patients become eager to take advantage of the convenience of digital healthcare.
Mastering Diabetes Naturally

I have been listening to the Food Matters Total Wellness Summit online and one of the interviews was with the two authors of the New York Times bestselling book Mastering Diabetes. Cyrus Khambatta and Robby Barbaro have degrees in nutritional biochemistry and public health (respectively) and are both Type 1 diabetics with firsthand experience on […]
4 strategies for healthcare providers to make virtual care practical for seniors

As telehealth becomes mainstream, seniors will be forced to adapt – but we as healthcare providers have a duty to make this process as seamless as possible, so one of our most vulnerable populations does not get left behind.
Will Amazon Move Into the Telehealth Space?
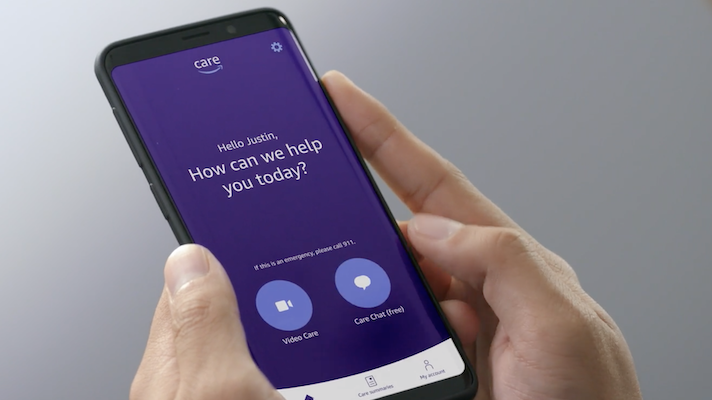
Amazon Care is rolling out to employees. Could customers be next?
How to Prepare for the COVID Vaccine

With vaccine availability now broadening to more groups, you may be wondering what steps you can take to prepare yourself for the shot(s). In this blog, I’ll describe some do’s and don’ts to consider. It’s important to note that these are not short-term solutions but ways to reach optimal health which will support the vaccine […]
COVID-19 One Year Later: What’s Next for Virtual Care?

The pandemic has created demand for remote patient care and telehealth. Could Lenovo’s virtual care solution interface with such digital tools and provide the health data providers need?
How American attitudes on telehealth have changed since the start of the pandemic

by Katie Adams Before the pandemic, 56.40 percent of Americans did not believe they could receive the same level of care from telehealth compared to in-person care, but recent polling shows 79.85 percent of Americans now say it is possible. Sykes surveyed 2,000 adults in March 2020 and March 2021 about their telehealth attitudes and experiences. Below […]
