Healthy Mitochondria Tips

“There is no amount of healthcare dollars that will improve our collective health status in the United States unless they are focused on mitochondrial health.” Casey Means, M.D. Ever wonder what keeps your body’s engines running smoothly day in and day out? Meet your mitochondria – the tiny yet mighty powerhouses of your cells! These little […]
Importance of Mitochondria for Overall Health

Importance of Mitochondria for Overall Health Type 2 Diabetes, Cardiovascular Disease, Neurodegenerative Diseases… there are so many chronic illnesses tied to poor mitochondrial function. Mitochondria are the power plants of our cells; they take the food we eat and turn it into energy called ATP. But they do more than just produce energy – they […]
Introducing the 30-Point Plant System to Power our Gut Microbiome

Introducing the 30-Point Plant System to Power our Gut Microbiome “There are no incurable diseases if one lives in harmony with nature.” Ann Wigmore Tweet Did you know that your gut microbiome is home to trillions of bacteria that play a crucial role in your health? With over 70% of your immune system residing in […]
Rethinking ‘Healthy’: The FDA’s New Definition

Rethinking ‘Healthy’: The FDA’s New Definition ‘Let food be thy medicine and medicine be thy food.’ Hippocrates Tweet Imagine walking through a grocery store, picking up a box of cereal labeled “healthy,” and feeling good about your choice. Now, imagine later discovering that the product is loaded with added sugars, refined grains, and artificial ingredients. […]
Powerhouses of Our Body: The Mitochondria
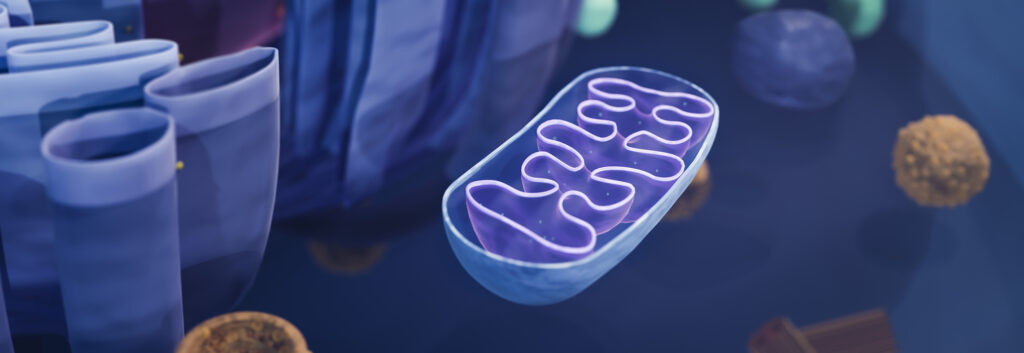
Powerhouses of Our Body: The Mitochondria Did you know your body is home to around 100,000 trillion mitochondria? That’s right – these tiny powerhouses are everywhere, working behind the scenes to keep you going! But what exactly are they, and why are they so important? In this blog, we’ll uncover the science of mitochondria and why […]
Chronic Kidney Disease Lifestyle Tips

Chronic Kidney Disease Lifestyle Tips “Your kidneys filter 200 liters (53 gallons) of fluid per day. Show them some love.” National Kidney Foundation Chronic kidney disease (CKD) is a growing global health concern, affecting millions of individuals worldwide. According to the National Centre for Health Statistics, CKD is responsible for 17.4 deaths over 100,000 worldwide. […]
8 Tips for Increasing Your Fiber During American Heart Month
8 Tips for Increasing Your Fiber During American Heart Month The proverb, “The tree that bends does not break,” highlights the importance of adaptability in the face of adversity. But if we think in a more literal sense: what is it that allows the tree to stand strong and tall and… flexible? The answer is […]
Exercise Snacking For Your Health

Exercise Snacking For Your Health “Just get 150 minutes of exercise per week” “Make sure you’re walking 10K steps a day” “Aim to get at least a 25-minute workout into your daily schedule.” There’s pressure to get enough exercise coming from all angles. Whether it’s the formal CDC recommendation of 150 minutes of physical activity […]
What Causes Chronic Kidney Disease?
What Causes Chronic Kidney Disease? Living with chronic kidney disease (CKD) can be tough because it keeps getting worse over time and can affect your quality of life as it progresses. Catching it early is super important because then you can do something about it sooner rather than later. Interestingly, CKD often remains hidden during […]
Sober October – A Month of Reflection and Renewal

Sober October – A Month of Reflection and Renewal If the events of this year have felt overwhelming, you’re certainly not alone. Many of us may have faced unprecedented challenges, from the shift to remote work to the inability to connect with friends and family. In such times of stress, we see that alcohol bottle […]
