The Future of Healthcare
Polymorphic Medicine™
Preface
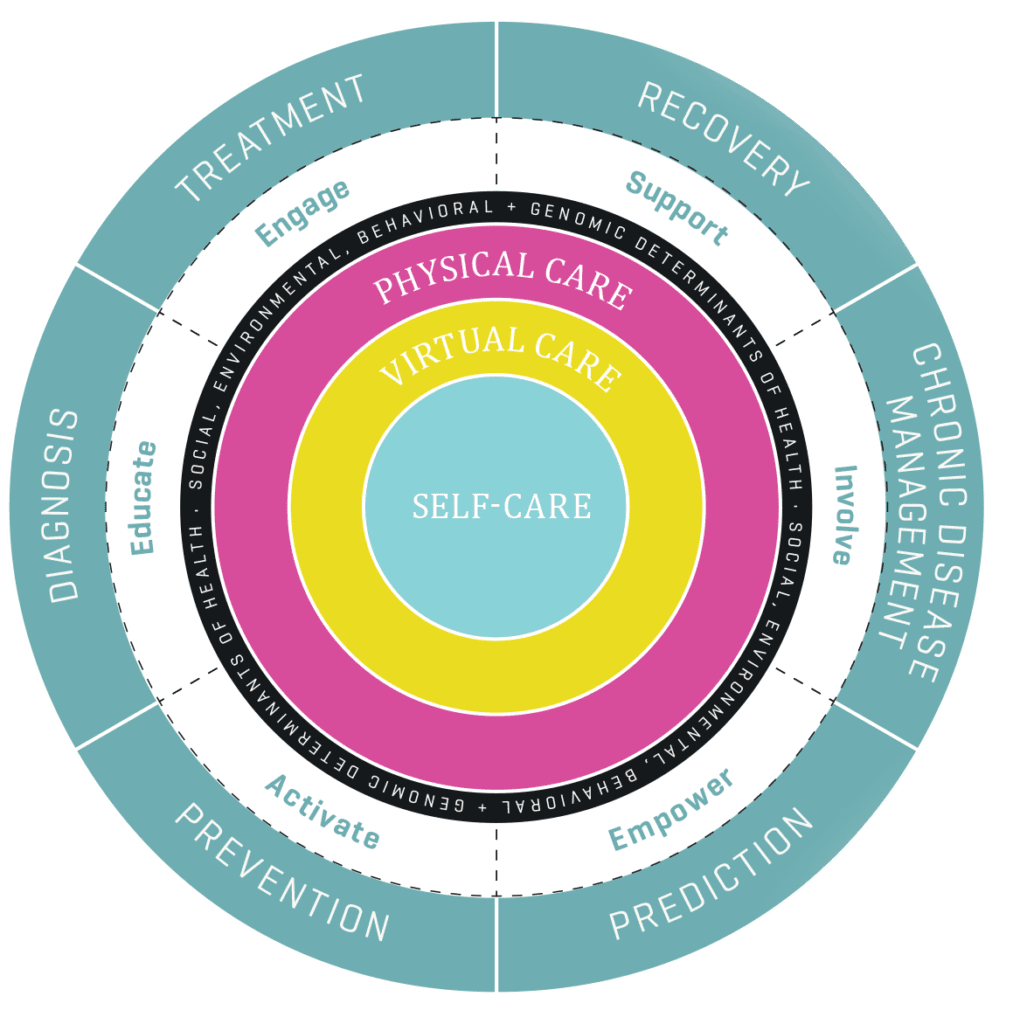
Polymorphic Medicine is a new approach to health and care encompassing a whole life health model, from self-care and disease prevention to treatment of acute and chronic conditions. It is the optimal blend of self-care, physical care, and virtual care — matching patient needs and preferences with available resources to maximize outcomes.
Polymorphic Medicine represents a paradigm shift towards the next evolution of healthcare. If the first decade of the 21st century was characterized by the “systemization” of healthcare with the introduction of electronic medical records, and the last decade saw the rise of genomic-based personalized medicine, we are now on the cusp of transitioning to the next phase — a re-humanization of healthcare with the system oriented around the individual, enabled by technology and informed by advanced analytics.
If COVID-19 has been the tipping point for the widespread adoption of virtual care and remote monitoring, the time is now for a new type of healthcare, one that is focused on reducing the overall burden of disease at a population level and supporting a person to better manage their own health at an individual level. This requires a level of personal responsibility and accountability by the individual, accompanied by a legislative environment that prioritizes the promotion of health, while discouraging policies that undermine it. And it requires a systematic digital and cultural transformation in the way that healthcare is designed, delivered, and experienced.
It is the optimal blend of self-care, physical care, and virtual care — matching patient needs and preferences with available resources to maximize outcomes.
It starts with informed and motivated self-care to prevent or reduce risk factors, supported by virtual care for timely access, convenience, and affordability. It promotes effective and efficient physical care to be accessed only when and where needed to optimize outcomes.
Polymorphism is the ability of medicine to take on multiple forms — not just delivered by physicians in a clinical setting addressing sick patients but representing an holistic, integrative approach to health, care and wellness that meets the individual where they are now, both physically and emotionally, where they live, work, learn, play, and pray. It transcends the clinical setting and is firmly rooted in the social, environmental, and behavioral determinants of health and it is our belief that good health is co-created by individuals, the system that supports them, and the environment in which they live.
Healthcare is no longer limited by time and place. Health is life. And healthcare can be part of everyday life. That is the vision of Polymorphic Medicine. That is the mission of Hippo Technologies.
Introduction
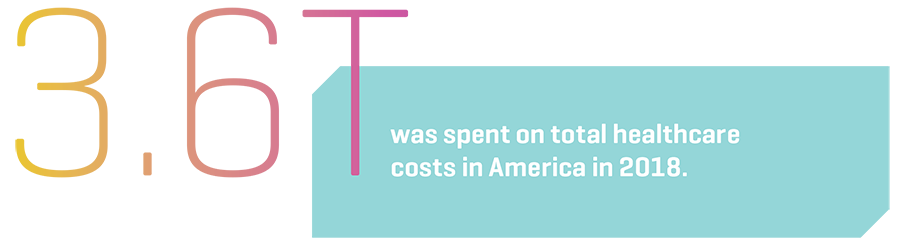
In 2018, total healthcare costs in America hit a new record of $3.6 trillion, according to the federal government. That’s approximately 18 percent of the country’s total gross domestic product (GDP), which translates to an average of about $11,000 per person.5
Amazingly, relative to the size of the economy, healthcare costs in the U.S. have exploded from five percent of GDP in 1960 to 18 percent in 2018.5 And according to the Centers for Medicare and Medicaid Services (CMS) it is only going to get worse as they project that by 2028 such costs will rise to $6.2 trillion, which is about $18,000 per person which will represent roughly 20 percent of GDP.5 To put things in perspective, our national healthcare bill far exceeds all of the other things we spend money on, including food, clothes, housing, or even our military.
Luckily for many of us, the cost of healthcare is not equally distributed — not by a long shot! Meaning that we each don’t spend $11,000 on healthcare.
Instead, a small number of Americans run up most of the bill – in the healthcare field these people are referred to as “super-users” or “frequent fliers”. In fact, healthcare costs are so concentrated that 5% of Americans account for 50% of total medical costs whereas the average American only spends roughly $1,000 per year on medical costs. Another way to look at it is this — if the population of the country was 20 people, we would be spending the same amount on the costliest patient as we would be spending on the other 19 combined.1
An article in the Atlantic gave some interesting insights into these “super-users”:
“Truth is, there is no single group of sick people to blame for the United States’ high health care bills. Among the Five Percent, there is no “them.” Instead, the sickest five percent of Americans are drawn from all Americans — the young, the old, the chronically ill, and the temporarily injured alike.
There’s a great deal of turnover: In any given year, half of the Five Percenters will get better and drop out of the bracket. Fact is, the chronic conditions plaguing high-cost patients are quite common lower down on the cost scale, too. And no one has figured out how to tell when a stable, low-cost diabetic will jump into needing intense care.
If this spending disparity were a recent phenomenon, researchers might have an easier time picking out a cause. But studies show this distribution has persisted since the 1960s, and possibly even further — before the big entitlement programs of Medicare and Medicaid were founded.”1
Dr. Donald Berwick, the former head of the Centers for Medicare and Medicaid Services under President Obama summed up the root cause of all of this very succinctly when he said, “The healthcare system as a whole is out of balance. We put far more into hospital care than we do keeping people from having to be in the hospital.”3
Many healthcare experts believe that the key to decreasing healthcare expenditures is to reduce the costs to the “super-users”. This can be done in a couple of ways — either by figuring out how to make care less costly via better management or to keep those super-users from requiring care in the first place via preventative medicine.
“The healthcare system as a whole is out of balance. We put far more into hospital care than we do keeping people from having to be in the hospital.”
Dr. Donald Berwick
Former head of the Centers for Medicare and Medicaid Services

Many experts in the public health arena believe the impact of physician and patient behavior to healthcare costs is far exceeded by the health effects of what are known as “social determinants”. Factors such as poverty, homelessness, lack of nutrition, crime, environmental issues, and the chronic explosion of diseases such as arthritis and degenerative illnesses of the nervous system which are the inevitable results of aging all play their part.
However, by failing to take responsibility for and effectively manage the deteriorating functionality of our own bodies as we grow older, we are denying the unavoidable and the inevitable. This lack of responsibility just ends up driving many needlessly into an extraordinarily costly healthcare system.
What’s true is this – the current system is broken and devoid of both self-responsibility and self-care at scale. The global pandemic in which we find ourselves has shone a bright spotlight on how fragile the system is, in terms of health disparities and shortcoming in capacity of care.
You may be asking yourself, “Ok, so where do we go from here?” Well, what we need to do is to stop addressing the symptoms and start addressing the root cause or else we are doomed to repeat the cycle that has occurred since the 1960s. What we need is a new approach and that is the Polymorphic approach to health.

How do you solve the problem of healthcare?
Problem solving has three important steps:
- Focus on the right goal by asking the right question — define the problem and identify the root cause; do not confuse cause with symptoms.
- Describe the ideal solution in detail — from Healthcare to Lifecare.
- Design a plan of implementation which works back from the future state to the present problem — a Polymorphic approach to problem solving.
1. Focus on the right goal
There’s an old adage: don’t build a better mousetrap, just eliminate the mice. The elimination of mice is the goal, a mousetrap is only a means to an end. The same applies to healthcare. As a system, we repeatedly focus on the delivery model (it is understandable, conventional, financially rewarding to many stakeholders yet insufficient for the creation of a healthy population) and we continue to bypass root cause discovery and intervention. We know the major cause — lifestyles arising from the socioeconomic, environmental, and behavioral determinants of health — but devote far more resources to modifying the conventional delivery systems.
The clear priority should be the conscious, highly synchronized modification of lifestyles and personal choices which create health and disease as the basis for health transformation. With that as the goal, we can connect with current assets and work back to devise the means to achieve this goal. We know that the immediate need is to optimize current assets to improve the delivery of care. We must use the goal of wellness as the guiding force as we migrate from present to future.
More specifically, the goal should be finding a long-term healthy and sustainable lifestyle so that our actions today are an investment in our future health.
It is important to note that every advanced country has made the same fundamental mistakes when it comes to healthcare — they violated each of the basic steps of problem solving as described above:
- They failed to accurately define the root cause and focused on the symptoms of the problem rather than the root cause itself.
- They failed to identify the ideal solutions in detail; and
- They worked instead from a failed hodgepodge of the present in the hope of a solution materializing in the future.

We all know that hope is not a plan: in the face of serious threat, it is a danger. Unsurprisingly, the symptoms and associated costs became worse despite numerous broad, complex, and expensive interventions by governments and health systems over decades. The United States is the best example of this failed approach. Other nations are not far behind on this road to failure.
On the other hand, there are populations who have taken a different approach to health, wellness, and longevity that rely on addressing root causes rather than symptoms. Take for example, the Japanese, and particularly those who live on the island of Okinawa, where there are 24.55 people over the age of 100 for every 100,000 inhabitants — far more than the global average.”1 Those who study the longevity of those on the island attribute one of the main reasons (others being diet, a simple life in the outdoors, green tea and the warm climate) to the ikigai that guides their life. According to those who live on the island, the ikigai is “the reason we get up in the morning.”1 What is also true is that the people on the island take personal responsibility for their health in a variety of ways, some of which include:
- Staying physically active and doing what they love as long as their health permits.
- Instead of eating until they are full, they stop eating when their stomachs reach 80% capacity. This limits overeating and prevents drawn out digestive processes that speed up cellular oxidation.
- While there is no doubt they are hard-working people, what is also true is that they are also very skilled at being absorbed in a task by living in the moment (the practice of mindfulness).
- They are grateful and practice gratitude every day.
- They connect with nature as a way to recharge their batteries and reduce stress.
- Smiling and having fun is critical. Those who live on the island are constantly celebrating — dancing, music, and song are a big part of their lives.
The point is this, any attempts at healthcare transformation need to address the symptoms and root cause simultaneously. It must be a two pronged, highly coordinated attack and in the words of Apple we need to “Think different” if we want to achieve different outcomes (Einstein would have had a field day with the current healthcare system).
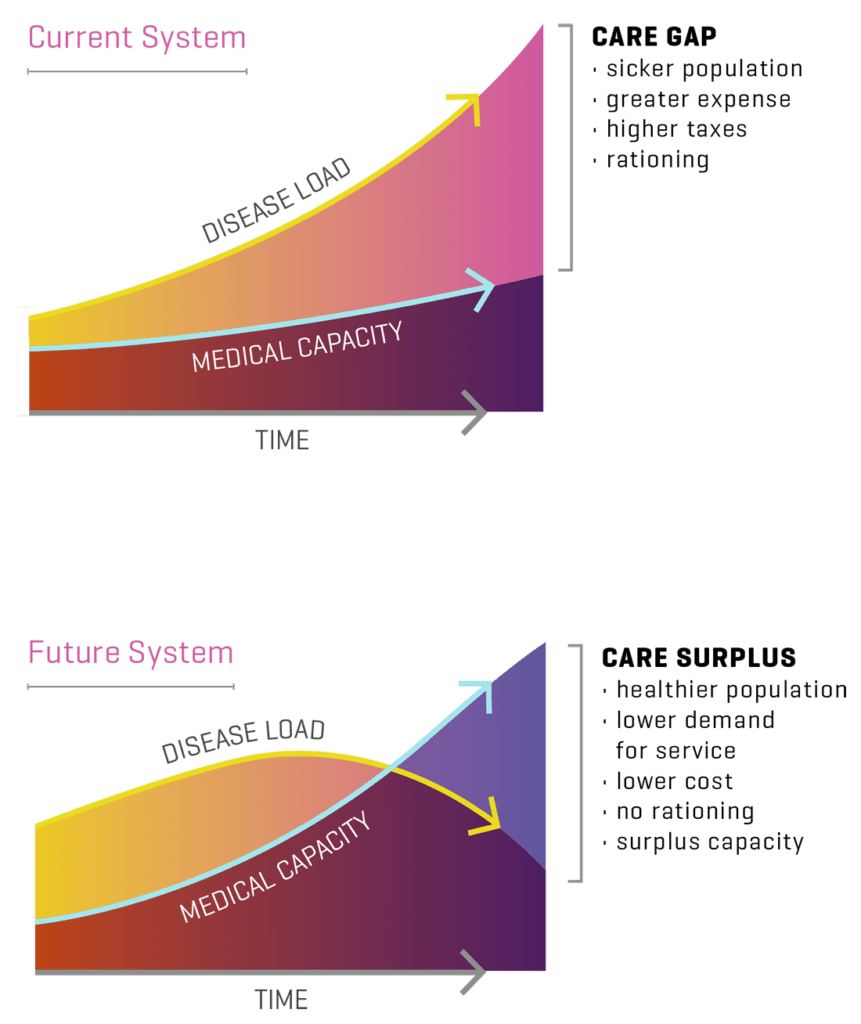
Our current focus is only on one prong — the Model of Care — which by itself, no matter how successfully designed and executed, will ultimately fail to meet the needs of the public. The multipliers of chronic disease will always generate demand for services greater than the ability to provide them. Reducing demand must go hand in hand with increasing supply. This is the most valuable lesson for those looking to transform their health system. It provides a clear warning as well as a great opportunity.
Address the root cause, not the symptoms.

The problem is the “disease load” of a given country — the number and severity of the diseases present in a country, state, or community. The disease load is the source of the demand for services, which is expressed as the symptoms we are all too familiar with, such as stroke, heart attack and so forth. The urgent nature of these symptoms, and the conventional approaches to them have understandably deflected our attention from the root cause. Eighty percent of resources are expended on the management and consequences of chronic disease, most of which arise from lifestyle choices. The forces which shape lifestyle choices are powerful and largely beyond the reach of conventional medical practice. It is estimated that standard medical practice can only affect lifestyle choice by 10% — the rest is driven by social, environmental, behavioral, and genomic determinants of health.
True, fundamental prevention occurs in daily life, not the Doctor’s office. The crucial task of modifying lifestyles then, is the primary purview and responsibility of the leaders of society. We need a comprehensive plan for lifestyle change, which is owned and driven by political and social leadership and supported by a universal model of care – an approach that we call “Health in All Policies”. This requires a unified, highly integrated, and orchestrated plan for wellness, which forms the basis for Polymorphic Medicine.
2. Describe the solution in detail: From Healthcare to Lifecare
Lifestyle drives 80% of disease and chronic disease drives 80% of cost, so lifestyles are at the center of both the problem and the solution. Lifestyles are driven predominately by socioeconomic factors so the interventions must be directed at those customs and practices which shape behaviors. While physician and hospital-based methods are traditionally used to change lifestyle/patient behaviors, these methods have failed to materially change the health of a population. It will take socioeconomic and political forces to change social behaviors.
The desired end state is a healthy individual who understands his or her personal health risks and successfully manages them through healthy lifestyle choices, which are easy to practice in a social and physical environment conducive to health, and enabled by a highly personalized support system. This future system is fully digitalized and layered with both automation (machine learning) and personal team support. It begins with the individual at home and works on a real-time basis. Virtual and physical care are seamlessly blended, based on the needs of the patient and their family. Much of chronic disease is successfully prevented, and that which presents is managed efficiently to lower levels of acuity. Medical care is delivered by teams in person and virtually to improve timely access and medical outcomes, and ultimately reduce costs.
This ideal future state based on the precepts of Polymorphic Medicine is within the grasp of enlightened communities and governments.
Imagine a society where everyone “knows their numbers” — they know their health risks and they know how to manage or eliminate these risks. Importantly, they take personal responsibility and accountability for doing so. Imagine a society where doing the healthy thing is easy and doing the wrong thing is emotionally, physically, and socially difficult. Imagine a society where the socioeconomic forces that truly drive behavior work in unison to create a healthy population. Imagine individuals and families who are ready, activated and informed to make the right health choices at the moments of decision. Imagine a society where the inner lives of people drive them to be healthy and the environments where they live, work, learn, play, and pray are strongly pre-disposed to health.
This ideal future state based on the precepts of Polymorphic Medicine is within the grasp of enlightened communities and governments. Wellness should be the primary goal, and programs such as delivery systems and payment models, governmental policies for education, commerce and public life are a means to that end. As a result, health becomes not a service or program, it becomes a way of life — a new tradition which unlocks the potential of its people.
Motivated, informed self-care is supported by a complete environment conducive to health at work, school, home, church, and places of recreation. Public policy supports all sectors to facilitate good health choices and discourage bad ones. Behaviors are developed and sustained for very powerful reasons. Information alone is insufficient to change them. These reasons must be fully understood, accepted by the individual and acted upon. Meaningful and constant healthy lifestyle choices must be embedded in the full social environment to overcome those forces which gave birth to unhealthy choices.
Health protective policies have been implemented in the past. The policies create healthier communities and countries.
Self-care, in this context, is supported by a hyper secure private health portal that identifies individual health risks and the means to avoid or minimize them, coupled with a steady stream of feedback on choices, decision support for the right decisions and sophisticated motivation to implement constant improvement in the individual’s health status. Effective private health decisions hinge in large part on social acceptance and feasibility of action. This will require authentic leadership which consistently describes the nature of our healthcare problem and the urgent reasons for change: the progressive bankruptcy of the country, the subsequent underfunding of all social support programs like Social Security, Medicare, and Medicaid, and critical functions like national defense, and national infrastructure. The financial crisis pits programs and parties against one another in a zero sum game and paralyzes our government. For the first time, we will have to think our way out of a problem rather than buy our way out. It is our task to clearly and compellingly describe the problem, the related consequences and the set of solutions to solve it.
3. A polymorphic approach to problem solving
The plan for implementing Polymorphic Medicine should encompass social change on a national scale and will require all of the elements of change management, with a special emphasis on social and political factors. Creating a compelling case for change and personal responsibility for a healthy lifestyle is the key to Polymorphic Medicine and is its principal challenge. A pervasive communication plan embedded in all forms of policymaking, education and media from the start is essential.
Acceptance of the plan and compliance with it is an art which must be perfected. Good ideas which aren’t accepted will fail. Policies at work, in school, in commerce and government must make good choices easy and poor choices difficult. Only when we achieve acceptance can we make it more difficult to do the wrong things and easier to do the right things. Success ultimately occurs when a healthy lifestyle is part of individual and national identity.
Here are just a few examples of how embedding health in various forms of life can have a dramatic impact:
1. Embed Health in policies. Over the years there have been countless examples of health being embedded in policymaking, such as:
- The introduction of mandatory seat belts and the impact that had on reducing deaths from car accidents.
- The sugar tax imposed by certain governments on soft drinks manufacturers.
- The ban on smoking in public and confined spaces, and the impact that had on population health.
- Mandating dietary information on product labeling and calorie information on restaurant menus.
- What’s true is that the examples above are only scratching the surface of what is possible.
However, we can go even further by making informed choices possible and attractive by being strategic with respect to positioning, presentation, and pricing. For example, one idea may be to cross reference bar codes and checkout receipts which load to individual health records with personal goals for real time feedback/decision support and behavior modification.
2. Embed Health in educational content. Incorporate health information into curricula holistically (across math, science, geography, history, and literature, not just limited to home economics). The next generation will be inculcated with the knowledge of the healthy life and predisposed to put knowledge into practice. At least when activated, they will know what to do, and importantly, why to do it.
Also, education at home is critical as parents must serve as role models to their children. For example, by cultivating the habit of cooking fresh and healthy meals at home as a means of cultivating a healthy lifestyle. Parents who lead by example through their daily routines in healthy behavior will create deep education for generations to come.
3. Embed Health in all media. Tell stories that appeal to a higher purpose: save our children, prevent unnecessary suffering. Infuse a sense of patriotism in our storytelling (it’s patriotic to be healthy, we all need to do our bit to contribute to a healthier community and society). Leverage faith-based communities and their universal message of “all things in moderation” to address addictive behaviors. Manage the image of health through emulation, leveraging sporting figures, celebrities, royalty, political and religious leaders. Ensure that everyone is singing from the same hymn sheet when it comes to health and telling a consistent message. Make social media platforms accountable for distributing fake health news that flies in the face of clinical evidence base.
4. Provide universal access to virtual care. It has taken a global pandemic to act as the tipping point for telehealth to become mainstream. Remote monitoring is well underway. The opportunity before us is to expand that kind of support to other lifestyle challenges and integrate it in ways that lead the world in a wellness way of life.

Conclusion
The transition to Polymorphic Medicine will require true innovation as well as a change in mindset. The digital transformation of healthcare and the fundamental drivers of health and disease will require social innovation, much more a social grass roots movement than policy; a movement grounded in science but led by political and social institutions. Change management on a national scale will require popular acceptance to succeed. There is a science to change management. There is both an art and a discipline to discover and solve points of resistance, especially unspoken beliefs, goals, and commitments. Healthcare change is assisted by its own merit — the goal of a long and healthy life and the opportunity to achieve full individual potential; a movement grounded in compassion for others and a love of life and of family. In the end however, the prime requisite is a clear, compelling vision and the courage to pursue it.
That is not to say that the current model of care should be completely abandoned. It can and will be improved. Those in medicine and the public expect and deserve better. But it is equally vital to understand the problem in its full context. The delivery of health services alone will not solve the symptoms of a deeper problem, the root cause of the national health threat befalling countries around the world. The symptoms are powerful, immediate and compelling; the numerous acute medical problems and the many faces of chronic disease — heart attack, heart failure, lung disease, stroke, kidney failure, blindness, joint disease, and cancer — demand action. That said, we cannot be ensnared in the same trap of a singular focus on the symptoms at the expense of a focus on the cause of the problems. We must address both concurrently.
Proof that these chronic conditions are rooted in lifestyle is apparent when comparing health 50 years ago to today. There was (almost) no diabetes or hypertension in children, and cancer rates were significantly lower. Instead, people died from bad sanitation.
Put simply, health transformation has two aspects — Sick Care, which is the responsibility of the medical establishment, and Well Care or Wellness which is the responsibility of societal leaders. The two are joined at the level of the individual by digital health, and the programs, policies, and environments that promote a healthy lifestyle. The addition of national lifestyle intervention will ultimately reduce total demand for services and allow the improved medical system to put demand and supply in balance. That is the opportunity afforded by a transition to Polymorphic Medicine. That is our task at hand.

Patrick Quinlan, MD is former CEO of Ochsner Health, one of America’s most progressive health systems, and current CEO of Hippo Technologies, Inc.
References
- https://www.theatlantic.com/theplatinumpatients/
- https://www.theatlantic.com/health/archive/2017/06/how-we-spend-3400000000000/530355/
- https://www.theatlantic.com/health/archive/2017/06/fixing-the-5-percent/532077/
- García, H., Miralles, F., & Cleary, H. (2017). Ikigai: The Japanese Secret to a Long and Happy Life. New York, New York: Penguin Books.
- https://www.pgpf.org/blog/2020/04/why-are-americans-paying-more-for-healthcare