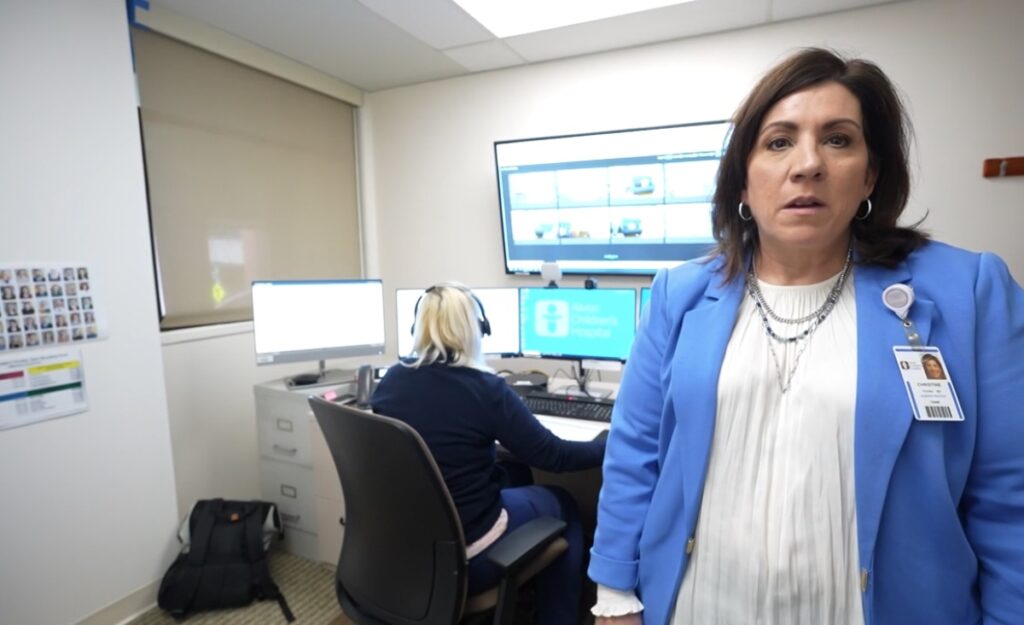
How virtual health tools are making hospital rooms ‘smart’

In an effort to reduce patient harm and support staff efficiency, Virtua Health is modernizing the hospital room with virtual health tools, such as cameras and sensors.
Extend, don’t reverse, virtual health care options

Elon Musk, the nation’s cost-cutter in chief, should consider telehealth’s return on investment, not just its price tag.
Akron Children’s is using ‘virtual’ nurses. Here’s what that means for patients:
For some patients staying at Akron Children’s Hospital and their families, an additional member of the care team is now available to provide updates and ask questions through their in-room monitors.
Unifying telemedicine efforts can help health systems succeed with virtual care

That’s the message Teladoc Health’s Scott Wilson and two colleagues from Valley Health System will be delivering at HIMSS25. Wilson offers a preview of the session, with tips for realizing value from telehealth.
Understanding the Legal Pitfalls of Virtual Second Opinions: What You Need to Know

Virtual medical second opinion (VSO) programs continue to roll out across the country, delivering expert recommendations to better help patients’ diagnoses or treatment options. These VSO programs can offer immense value to patients and their local treating doctors by leveraging the deep expertise of specialists and exporting it to rural communities and geographies that lack such sub-specialty expertise.
Why are pharma, medical device and DTx companies investing in telemedicine?
One virtual care CEO says telehealth is improving care for rare and complex diseases, helping compounding pharmacists – and continually improving with artificial intelligence.
AI Virtual Therapists Could Improve Mental Health Care, Studies Find

New research shows that artificial intelligence (AI) and virtual reality (VR) goggles could revolutionize therapy — helping patients overcome addiction and receive unbiased care.
Older adults’ digital health use varies by race, other factors

New research reveals that older adults use various digital health tools, including patient portals and telehealth platforms, but demographic factors shape utilization.
Tulane launches 24/7 virtual mental health support for students
As part of its ongoing commitment to student mental health and well-being, Tulane is launching a new telehealth service that will offer behavioral health care as well as crisis management and mental health coaching for students.
Telehealth helps people get health care, but access may soon be in limbo

Virtual doctor visits have been a game changer for improving access, especially in rural areas
