Assessing the value of a command center model in large health care delivery systems
Command centers can drive health care efficiency
In the evolving health care landscape, centralized command centers can provide a transformative solution for hospital systems. These hubs of coordination and communication offer opportunities for commercial and federal health agencies to enhance patient care by streamlining operations and working to ensure that every resource—from specialist availability to bed occupancy—can be utilized with optimal efficiency.
What are command centers
Command centers are inspired by air traffic control and mission control at NASA—and they look the part. Hospitals or systems can customize a command center according to their own needs, but typically, large screens line the walls and dashboards share real-time data across partner hospitals. Most hospitals have 20 to 30 staff members sitting on the command center floor at a given time, depending on the center’s needs.1
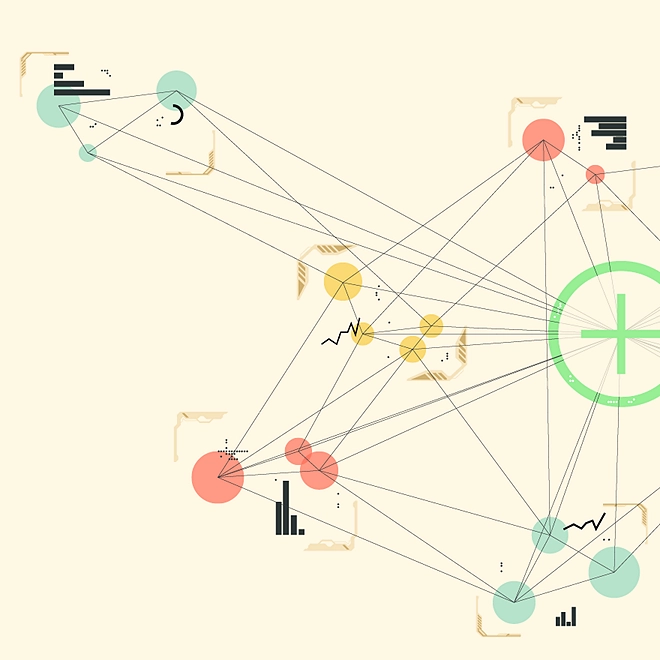
Command centers are the nerve center of a hospital, operating as centralized analytics hubs that monitor capacity, inventory, and patient flow. Many command centers begin with the goal of promoting patient safety and quality of care, compiling basic metrics from emergency rooms. Gradually, they can advance to tackle more complex problems like return on investments and addressing health inequities (figure 1).
Consider a recent example from Oregon Health and Sciences University. Before implementing a virtual command center, personnel used a whiteboard to manage the hospital system’s needs. At OHSU, a system comprising four hospitals, the whiteboard wasn’t keeping up with admissions. In 2016, OHSU was unable to accommodate 568 transfer patients; each was thus forced to rely on their care provider to locate an alternate facility with open beds and qualified specialists. The hospital system decided it needed to innovate. In 2017, OHSU adopted an electronic “mission control” command center. Within two years, they were referring 1,200 patients a year to partner facilities, almost double their 2017 numbers. OHSU’s new management system freed up enough beds to accept roughly 600 more transfer patients.2 The system was so successful at managing patient overflow that OHSU took over managing patients for the entire state during the COVID-19 pandemic.3
Hospital command centers—which use data analytics to track resources, patients, and special requirements—are improving the efficiency of major hospital systems. Tampa General Hospital credits its command center with saving US$40 million in the first 13 months of operation, cutting emergency-room diversions by 25%, and reducing the average length of stays by the equivalent of adding 30 beds.4
Command centers represent a natural opportunity for federal health systems, which manage vast patient volume and draw resources from wide regional networks. They can help hospitals triage efficiently, track resources, and facilitate patient transfers—saving precious provider time and lives. Some hospitals adopted command centers specifically to deal with the pandemic.5 Others adopted them earlier and have come to rely on these systems for resilience during public emergencies like hurricanes or the 2023 pediatric respiratory syncytial virus surge.6
As the US population grows and ages, climate-related health emergencies, emerging antibiotic-resistant infections, and the ongoing addiction crisis are expected to put additional pressure on hospitals.7 Command centers can help ease that burden through real-time decision-making, coordination, communication, and predictive analytics, addressing challenges beyond just patient flow management.
Command centers: A blueprint for breakthrough performance
Hospital command centers can make sharing and monitoring of data and resources more efficient, responsive, and informed. The cost savings and improved patient outcomes, as seen at hospital networks like Johns Hopkins Health System and OHSU, could prove equally, if not more, impactful when implemented at the scale of federal health systems. By leveraging technology and shared leading practices, government could transform public health, making high-quality care accessible and affordable. Therefore, it’s important to establish a blueprint for the operation of command centers. This blueprint should outline the types of benefits that may be reaped with the help of a command center (figure 1).
Hospitals often customize technology to suit their needs. Johns Hopkins consolidated 14 different data flow servers into one easy-to-view hub for their command center.8 Another health system partnered with fire departments and ambulance services to automate advance notice of incoming patients.9 AdventHealth managers measure the ROI of command centers through the quality of patient experience while other hospitals measure how the command center saves them money.10 A command center is a powerful tool. Simple use cases put patients in beds and providers at bedsides. More complex cases are yet to be imagined.
Command centers in action
Tampa General Hospital
In 2018, Tampa General Hospital realized it needed a way to address its consistently high operating capacity. To improve patient flow and safety, leaders introduced a hospital command center. Modeled after existing programs at hospitals like Johns Hopkins and Humber River, the command center would be led by senior leaders in collaboration with a vendor partner, and sustained by front-line staff members like registered nurses, bed allocators, and transfer coordinators.
TGH’s command center was launched in 2019, just in time to respond to the COVID-19 pandemic.12 Overseeing a 1,000-bed level-1 trauma center, the command center integrates all aspects of the system’s electronic health records (EHR) into a central location in a standardized format, saving providers hours of time.13 Using automated visual displays, these dashboards update hospital analytics in real time to monitor information like capacity, status of patients in observation, and barriers to discharging patients.14
The results speak for themselves. The hospital cut 20,000 excess patient days, discharged patients more efficiently, and helped triage emergency room visitors.15 The US$40 million reduction in efficiencies repaid the investment within a year after implementation.16
Johns Hopkins Health System
Pioneers at the Johns Hopkins Health System began planning their command center in 2014, as an extension of existing work groups focused on patient flow.18 The team included transfer line staff, admissions support, lifeline support, and bed managers, all of whom report to a medical director.
The system informs decisions. For example, if multiple stroke patients need one MRI machine, a physician can quickly compare each patient and sort them by level of deterioration. If a patient has multiple tests to run, the hospital can try to consolidate them into one trip, instead of returning to the bed each time. Hopkins also uses their command center to predict future patient volumes.19
The commitment to enhance patient experience is a crucial aspect of the command center’s functionality. At Hopkins, the command center personnel dedicate a specific screen to maintain a live feed from the waiting room.20 This practice serves as a constant reminder of the individuals they are ultimately serving and underscores the importance of patient-centered care.
Johns Hopkins’ results include:
- Enhanced proactive capacity management, boosting occupancy rates from 85% to 92%, despite a decrease in patient delays21
- A 46% improvement in accepting patients with complex medical conditions22
- A 38% reduction in time to assign beds, accelerating the process by 3.5 hours after the decision to admit23
- An 83% reduction in operating room transfer delays after the procedure24
- Generated US$16 million in annual revenue25
The transition was incremental, and setting up the command center took some time.26 But the results improved patient care and increased revenue for the health system, providing resources to further improve the patient experience.
Regional command center partnerships in play
To enhance health care service delivery, private hospital systems are increasingly leveraging regional partnerships to effectively manage resources, staffing, and bed capacity. This approach not only streamlines operations but also improves patient outcomes by ensuring that hospitals are well-equipped and adequately staffed to handle varying levels of patient care needs. Below are examples of how this strategy is being implemented in practice.
- OHSU, General Electric HealthCare, and Apprise (the Hospital Association of Oregon) implemented a statewide capacity-monitoring system during the COVID-19 pandemic.27 This program, using a dashboard that monitored bed availability and ventilator resources, allowed for rapid surveillance of the state’s 62 hospitals.28 The system worked. According to the Commonwealth Fund’s data set tracking days of high intensive care unit (ICU) stress across the United States during the pandemic, Oregon’s ICUs were overwhelmed for only 16 days between August 2020 and March 2022.29 In contrast, a third of states experienced between 150 and 566 days of overstressed units.30
- Tampa General Hospital helped set up a near-real-time Florida Capacity System across 51 hospitals in West Florida to manage beds, equipment, and hospital census numbers using command center tools.31
- The Halifax Infirmary site was the start of Nova Scotia’s “Action for Health.” This strategic initiative aims to increase efficiency of care delivery and experiences across Nova Scotia.32 As part of this action plan, they launched a command center named as Care Coordination Centre. It aims to increase efficiency, improve communication between clinics and higher care, and proactively improve health in the community, and eventually expand provincewide.33
Developing common command center capabilities
Common themes emerged from our interviews on how to create, implement, and sustain a digital command center. Figure 2 shows how a regional command center advances from basic to intricate tasks, through progressive levels of complexity, and expanding scope and scale. Such a virtual health support network enhances accessibility, convenience, and the overall experience of health care delivery and reception. When their potential becomes clear, hospitals can expand command centers to manage tasks like ICU prioritization, surgical scheduling, and infectious disease monitoring.
