By Oleg Bestsennyy, Greg Gilbert, Alex Harris, and Jennifer Rost
Telehealth has helped expand access to care at a time when the pandemic has severely restricted patients’ ability to see their doctors. Actions taken by healthcare leaders today will determine if the full potential of telehealth is realized after the crisis has passed.
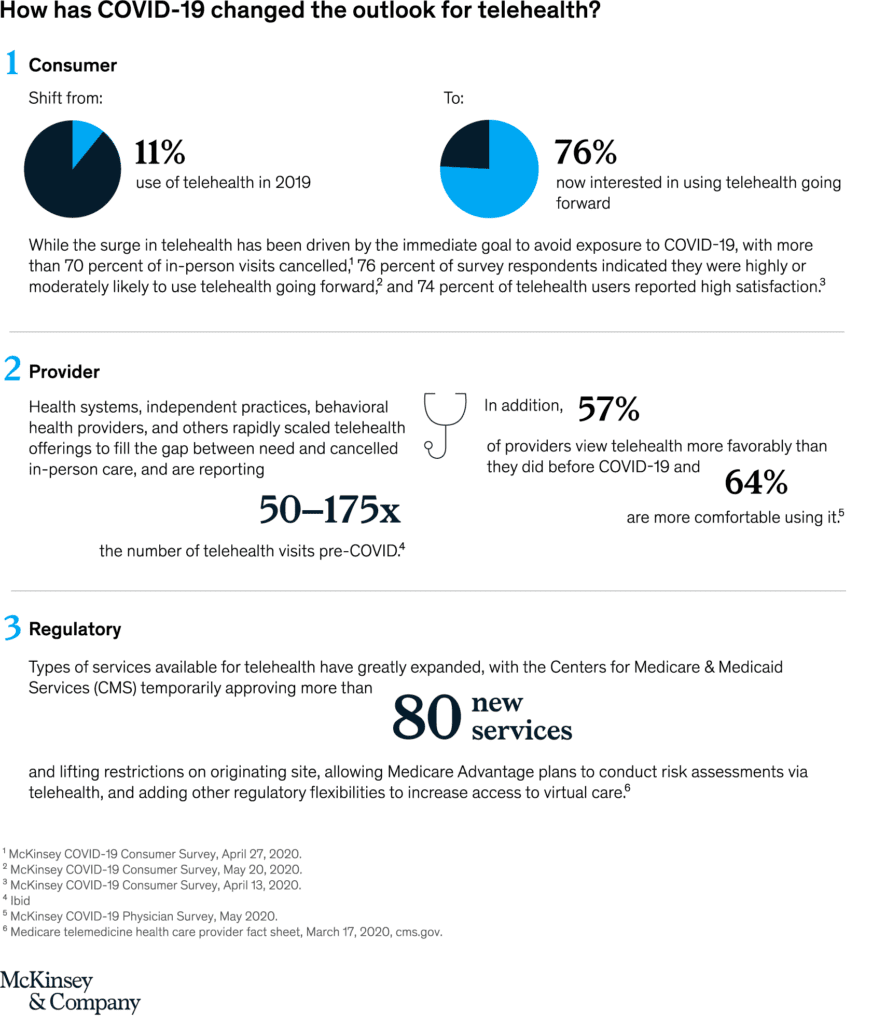
COVID-19 has caused a massive acceleration in the use of telehealth. Consumer adoption has skyrocketed, from 11 percent of US consumers using telehealth in 2019 to 46 percent of consumers now using telehealth to replace cancelled healthcare visits.1 Providers have rapidly scaled offerings and are seeing 50 to 175 times2 3 4 the number of patients via telehealth than they did before. Pre-COVID-19, the total annual revenues of US telehealth players were an estimated $3 billion, with the largest vendors focused in the “virtual urgent care” segment: helping consumers get on-demand instant telehealth visits with physicians (most likely, with a physician they have no relationship with).5 With the acceleration of consumer and provider adoption of telehealth and extension of telehealth beyond virtual urgent care, up to $250 billion of current US healthcare spend could potentially be virtualized.6
This shift is not inevitable. It will require new ways of working for a broad set of providers, step-change improvements in information exchange, and broadening access and integration of technology. The potential impact is improved convenience and access to care, better patient outcomes, and a more efficient healthcare system. Healthcare players may consider moves now that support such a shift and improve their future position.
Telehealth has surged under COVID-19
Many of these dynamics are likely to be in place for at least the next 12 to 18 months, as concerns about COVID-19 remain until a vaccine is widely available. During this period, consumers’ preferences for care access will continue to evolve, and virtual health could become more deeply embedded into the care delivery system.
However, challenges remain. Our research indicates providers’ concerns about telehealth include security, workflow integration, effectiveness compared with in-person visits, and the future for reimbursement.7 Similarly, there is a gap between consumers’ interest in telehealth (76 percent) and actual usage (46 percent). Factors such as lack of awareness of telehealth offerings, education on types of care needs that could be met virtually, and understanding of insurance coverage are some of the drivers of this gap.8
What is the full potential for telehealth and virtual care?
We identified five models for virtual or virtually enabled non-acute care and analyzed the full potential of healthcare volume and spend that could be delivered this way. These models of virtual care have increasing requirements to engage broader and broader portions of the healthcare delivery system, going from offering one-off urgent visits, to building omnichannel care models that deliver a large portion of office visits virtually or near virtually, to embedding virtual services in home care models. They include:
- On-demand virtual urgent care as an alternative to lower acuity emergency department (ED) visits, urgent care visits, and after-hours consultations. These care needs are the most common telehealth use cases today among payers. This allows a consumer to remotely consult on demand with an unknown provider to address immediate concerns (such as an acute sinusitis) and avoid a trip to the ED or an urgent care center. Such usage could be further scaled to address a larger portion of low acuity visits previously seen in EDs.
- Virtual office visits with an established provider for consults that do not require physical exams or concurrent procedures. Such visits can be primary care (such as chronic condition checks, colds, minor skin conditions), behavioral health (such as virtual psychotherapy sessions), and some specialty care (select follow-up visits such as virtual cardiac rehabilitation). An omnichannel care model that fully leverages virtual visits includes a mix of telehealth and in-person care with a consistent set of providers, improving patient convenience, access, and continuity of care. This model also enables clinicians to better manage patients with chronic conditions, with the support of remote patient monitoring, digital therapeutics, and digital coaching, in addition to virtual visits.
- Near-virtual office visits extend the opportunity for patients to conveniently access care outside a provider’s office, by combining virtual access to physician consults with “near home” sites for testing and immunizations, such as worksite clinics or retail clinics. For example, a virtual visit of a patient with flu or COVID-like symptoms could be followed up by a trip to a nearby retail clinic for a flu or COVID-19 test, with a subsequent follow-up virtual check-in with the primary care physician to consult on follow-on care.
- Virtual home health services leverage virtual visits, remote monitoring, and digital patient engagement tools to enable some of these services to be delivered remotely, such as a portion of an evaluation, patient and care giver education, physical therapy, occupational therapy, and speech therapy. Direct services, such as wound care and assistance with daily living routines, would still occur in person, but virtual home health services could enhance the patient’s and caregiver’s experience, extend the reach of home health providers, and improve connectivity with the broader care team. For example, a physical therapist could conduct virtual sessions with elderly patients at their home to improve their strength, balance, and endurance, and to advise them how to avoid physical hazards to reduce risk of falls.
- Tech-enabled home medication administration allows patients to shift receiving some infusible and injectable drugs from the clinic to the home. This shift can happen by leveraging remote monitoring to help manage patients and monitor symptoms, providing self-service tools for patient education (for example, training for self-administration), and providing telehealth oversight of staff (for example, an oncologist overseeing a nurse delivering chemotherapy to a patient at home and monitoring for side effects). This would be coupled with home delivery of the therapeutics.

Our claims-based analysis suggests that approximately 20 percent of all emergency room visits could potentially be avoided via virtual urgent care offerings, 24 percent of healthcare office visits and outpatient volume could be delivered virtually, and an additional 9 percent “near-virtually.” Furthermore, up to 35 percent of regular home health attendant services could be virtualized, and 2 percent of all outpatient volume could be shifted to the home setting, with tech-enabled medication administration. Overall, these changes add up to $250 billion in healthcare spend in 2020 that could be shifted to virtual or near-virtual care, or 20 percent of all office, outpatient, and home health spend across Medicare, Medicaid, and commercially insured populations.
Scaling telehealth does more than alleviate patient and provider concerns over the next 12 to 18 months until a COVID-19 vaccine is available. Telehealth can increase access to necessary care in areas with shortages, such as behavioral health, improve the patient experience, and improve health outcomes. Fundamentally, the integration of fully virtual and near-virtual health solutions brings care closer to home, increasing the convenience for patients to access care when they need it and the likelihood that they will take the right steps to manage their care. These solutions can also make healthcare more efficient; evidence prior to COVID-19 shows that telehealth solutions deployed for chronic populations can improve total cost of care by 2 to 3 percent.9 The actual opportunity is likely greater once stakeholders embed telehealth as the new normal (for example, driven by improved abilities to manage chronic patients, potential increases in provider productivity).
What actions should healthcare stakeholders take in the near term to shape this opportunity?
Actions payers could consider:
- Define a value-backed virtual health roadmap, taking a data-driven view to prioritize interventions that will improve outcomes for priority populations, and develop strategies to digitally enable end-to-care care journeys.
- Optimize provider networks and accelerate value-based contracting to incentivize telehealth. Define approaches (beyond the immediate COVID-19 response measures) to reimbursement and covered services, embed in contracting, and optimize networks and value-based models to include virtual health. Align incentives for using telehealth, particularly for chronic patients, with the shift to risk-based payment models.
- Build virtual health into new product designs to meet changing consumer preferences and demand for lower-cost plans. This new design may include virtual-first networks, digital front-door features (for example, e-triage), seamless “plug and play” capabilities to offer innovative digital solutions, and benefit coverage for at-home diagnostic kits.
- Integrate virtual health into the care delivery approach. Given the significant disruptions to providers, payers are reassessing their role in care delivery—from ownership of care delivery assets, value-based contracting, or anything in between. Consider options in virtual health (for example, platforms, digital-first providers) as a critical element of this approach.
- Reinforce the technology and analytics foundation that will be required to achieve the full potential of virtual health.
Actions health systems could consider:
- Accelerate development of an overall consumer-integrated “front door.” Consider what the integrated product will initially cover beyond what currently exists and integrate with what may have been put in place in response to COVID-19 (for example, e-triage, scheduling, clinic visits, record access).
- Segment the patient populations (for example, with specific chronic disease) and specialties whose remote interactions could be scaled with home-based diagnostics and equipment.
- Build the capabilities and incentives of the provider workforce to support virtual care (for example, workflow design, centralized scheduling, and continuing education); align benefit structure to drive adoption in line with health system and/or physician practice economics.
- Measure the value of virtual care by quantifying clinical outcomes, access improvement, and patient/provider satisfaction to drive advocacy and contracting for continued expanded coverage. Include the potential value from telehealth when contracting with payers for risk models to manage chronic patients.
- Consider strategies and rationale to go beyond “telehealth”/clinic visit replacement to drive growth in new markets and populations and scale other applications (for example, teleICU, post-acute care integration).
Actions investors and health services and technology firms could consider:
- Develop scenarios on how virtual health will evolve and when, including how usage evolved post-COVID-19, based on expected consumer preferences, reimbursement, CMS, and other regulations.
- Assess impact across virtual health solution/service types, developing a view of the opportunity for each solution/service type, including expected consumer/provider adoption, impact (for example, to outcomes, experience, affordability), and reimbursement.
- Develop potential options and define investment strategies based on the expected virtual health future (for example, combinations of existing players/platforms, linkages between in-person and virtual care offerings) and create sustainable value.
- Identify the assets and capabilities to implement these options, including specific assets or capabilities to best enable the play, and business models that will deliver attractive returns.
- Execute, execute, execute. The next normal will rapidly take hold, and those that can best anticipate its impact will create disproportionate value. Don’t underestimate the potential of network effect.
The window to act is now. The current crisis has demonstrated the relevance of telehealth and created an opening to modernize the care delivery system. This modernization will be achieved by embedding telehealth in the care continuum at scale. A $3 billion revenue market has the potential to grow to $250 billion. The seeds for success will be sown in the next few months during the COVID-19 crisis. Healthcare systems that come out ahead will be those who act decisively, invest to build capabilities at scale, work hard to rewire the care delivery model, and deliver distinctive high-quality care to consumers.
