The State of Virtual Care
In India
INTRODUCTION TO DISTANCE HEALING
In India the words Virtual Care translate to “healing at a distance” — which is synonymous with Telehealth and Telemedicine. Virtual Care can be considered a broader term in which healthcare providers use digital tools to communicate, deliver and monitor care to their patients remotely via phone, video, or connected device including wearables and sensors. Virtual Care can include everything from remote screening and diagnostics to treatment, post-op care, rehabilitation, second opinions, e-pharma services and the delivery of patient education and engagement. Remote diagnosis and treatment of patients using Virtual Care technologies can substantially improve healthcare. Improving access to specialists regardless of distance or demographics has the potential to substantially improve patient outcomes and population health in general.
India is the largest democratic country in the world, with over 1.4 billion people. It is a diverse, pluralistic, multilingual, and multi-ethnic society. Because of its abundant human capital, the Indian economy could be the engine of growth for the entire world. India received $34 billion in direct foreign investment in 2015. And yet, the country still faces numerous social and economic challenges including poverty, illiteracy, sanitation, gender inequality and lack of access to healthcare for all.
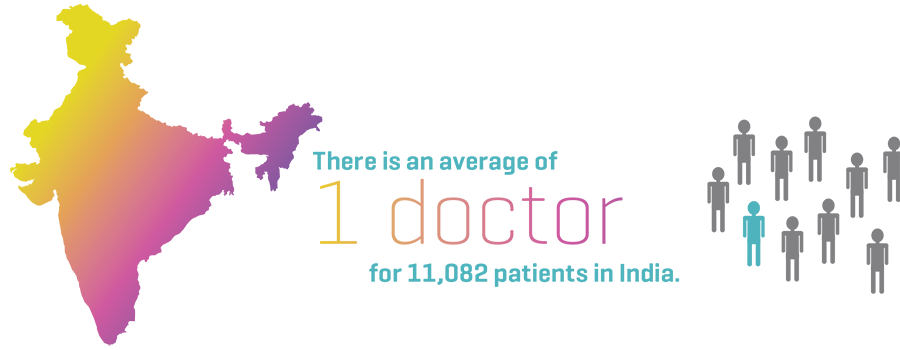
While public healthcare in India is free, affordable healthcare for all remains one of the biggest challenges facing India today. Continued under-investment in public health for years has led to facilities being under-staffed and under-equipped. The direct effect of low government spending on public health has resulted in high out-of-pocket (OOP) expenditure. High OOP payments are the main deterrent to citizens to access healthcare services, especially in rural areas. Several studies have shown that high OOP expenditure is one of the most important and contributing factors in pushing families and individuals into poverty. In India, 68% of the population still lives in rural areas. Rural healthcare systems are plagued with several problems including a severe shortage of healthcare professionals, lack of necessary medical supplies, as well as non-medical infrastructure such as electricity, clean water, logistics and finances. Approximately 60-80% of physician positions in various specialties are vacant in rural healthcare settings, while 75% of healthcare services and facilities are clustered around cities and towns, not to mention the massive resource gap of over 4 million healthcare workers. Thus, reforming healthcare in India is a daunting task.
Virtual Care is poised to transform the entire healthcare industry. People from rural areas travel hundreds of miles, often spending a month’s wages to see a physician. Remote diagnoses and access to quality healthcare at the primary level has the ability to save these patients time and money, which would in turn make them less likely to delay care. The benefits of Virtual Care extend to various stakeholders of the healthcare ecosystem, including:
- Patients, who experience greater convenience, more access, and lower costs.
- Doctors, nurses, and caregivers, who command more flexible schedules and improved access to patients and information.
- Healthcare leaders and administrators, who can lower overhead costs and expenses while boosting operational efficiency.

There are no straightforward solutions to India’s healthcare conundrum; however, leveraging India’s advances in the field of Information and Communications Technology (ICT) and applying them to healthcare delivery is an obvious solution to tackle this huge disparity. The widespread use of ICT in medicine has opened new horizons to improve healthcare across India.
A Telemedicine system in a small health center generally consists of a PC with customized medical software connected to a few medical diagnostic instruments, such as an ECG or X-ray machine or an X-ray scanner for scanning X-ray photos. Through this computer, digitized versions of patients’ medical images and diagnostic details (such as X-ray images and blood tests) are dispatched to specialist doctors through a satellite-based communication link. This information, in turn, is received at the specialist center where experienced doctors examine the reports, diagnose, interact with the patients (along with local doctors), and suggest appropriate treatment through videoconferencing. The entire system is relatively user-friendly, and only a short period of training is required for doctors at super-specialty centers and rural health centers to operate the system. Hospital technicians can take care of the operation and maintenance of the equipment.
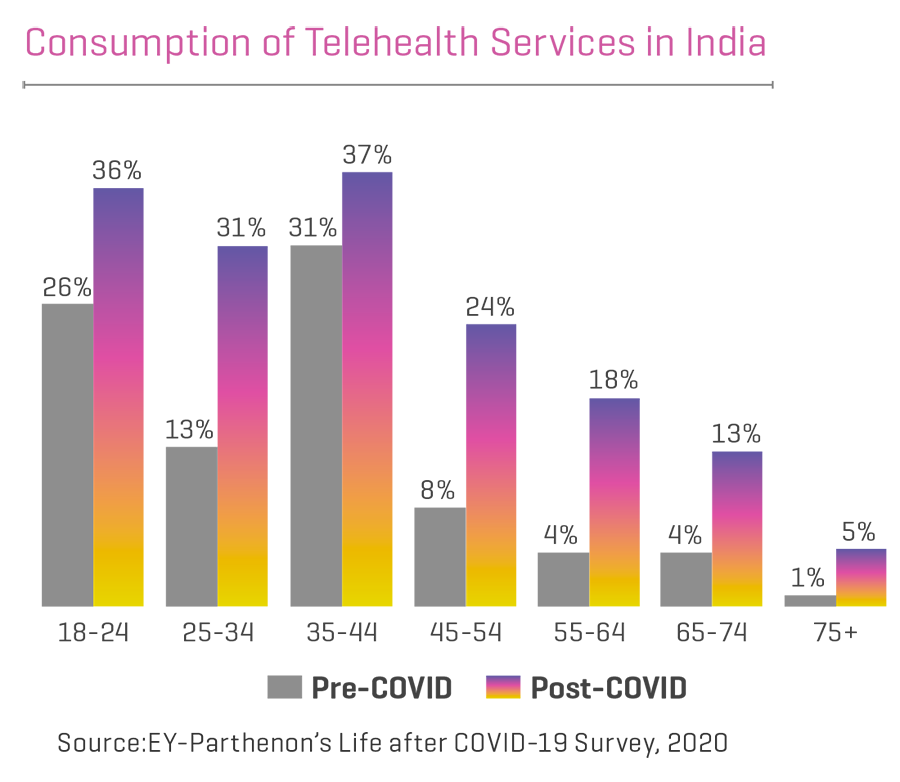
In the present scenario, the healthcare industry continues to evolve and adjust to the extraordinary demands of fighting the COVID-19 pandemic. The current crisis has given a boost to the proliferation of Virtual Care, but even in pre-COVID times, the healthcare sector was slowly gearing up for this next wave in care delivery. What COVID-19 did was help patients get acclimated to the digital health tools and services available. Once a hard sell, Virtual Care is now a much sought-after commodity.
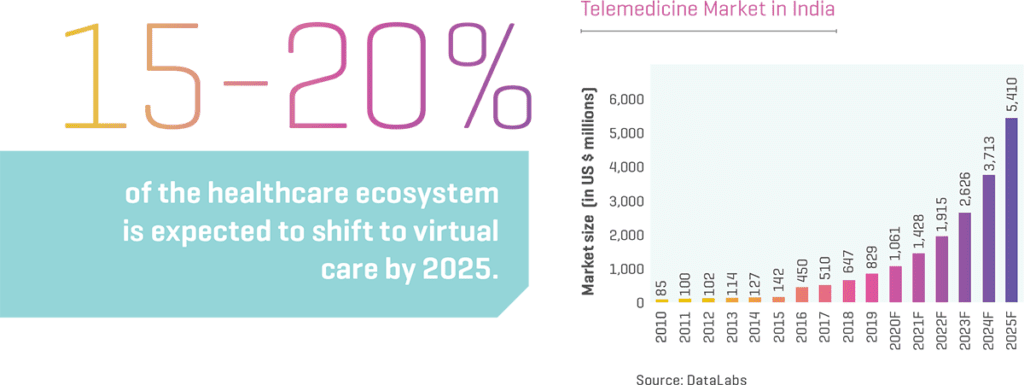
The Indian government is committed to providing equal access to quality healthcare for all, and digital health is a critical enabler for the overall transformation of the healthcare system. Mainstreaming Telemedicine will undoubtedly minimize inequities and barriers to access. Healthcare providers, such as hospitals and e-pharmacies, have integrated teleconsultation platforms and scaled–up their existing digital offerings. Teleconsultation and e–pharmacy platforms have exhibited a sharp rise in adoption by both doctors as well as patients. For example, Fortis Healthcare has witnessed a shift in outpatient department consultations with 10% of the pre-COVID-19 consultations moving to the teleconsultation platform. According to an EY-IPA study – ‘Healthcare goes mobile: Evolution of teleconsultation and e-pharmacy in the new Normal’ – the Virtual Care market in India is expected to grow at a compound annual growth rate (CAGR) of 31% for the period 2020-25 and reach US$5.5 billion, and 15-20% of the healthcare ecosystem is expected to shift to Virtual Care, across triaging, consults, remote monitoring, and home health, etc. India’s e-pharmacy market is projected to reach 10-12% of the overall pharmaceutical sales in the next five years driven by strong regulations, increased funding, and creation of digital infrastructure. Although it is difficult to predict the future beyond COVID-19, in India, it can be viewed as a significant inflection point in the use of Virtual Care across the nation, leading to 20%–25% adoption of teleconsultation.

THE BIRTH OF VIRTUAL CARE IN INDIA
You can trace the humble beginnings of Virtual Care in India back in 2001, when the ISRO (Indian Space Research Organization) and the Apollo Group of hospitals launched a pilot project at an acute care hospital in a village called Aragonda, 16km from Chittoor, (population 5,000) in Andhra Pradesh. This pilot project, led by ISRO and DIT, GOI (Department of Information Technology, Government of India), linked the Apollo Hospital in Chennai with Apollo Rural Hospital in the village. What began with simple web cameras and ISDN telephone lines in the village hospital, now has a state-of-the-art videoconferencing system and a VSAT (Very Small Aperture Terminal) satellite installed by ISRO. Coupled with this, was the Sriharikota Space Center project (130km from Chennai) which formed an important launchpad for ISRO in this field. The 2001 project was a significant step towards digitizing healthcare, and the effort was rightly applauded by the Ministry of External Affairs and MoH&FW (Ministry of Health and Family Welfare).
This further opened the door to DIT setting up standard Telemedicine practice guidelines, and the MoH&FW setting up a National Telemedicine Task Force over the next five years. Further projects in disease surveillance and management led to the creation of organizations like ONCONET (National Cancer Network) and NRTN (National Rural Telemedicine Network). In the past few years, ISRO’s Telemedicine network has expanded to connect 45 remote and rural hospitals, and 15 super specialty hospitals in varied geographical locations including the islands of Andaman, Nicobar and Lakshadweep, and the mountainous regions of Jammu and Kashmir.
VIRTUAL CARE INITIATIVES IN RURAL INDIA
There is a significant shortage of medical professionals in India. The training of healthcare professionals is time-consuming and expensive, and hence the doctor-patient ratio in India is expected to remain low for the foreseeable future. Virtual Care has been acknowledged as an attractive solution, and many initiatives are underway to tackle this disparity and provide equitable access to healthcare for all.
The MoH&FW has set up a National Telemedicine Portal for implementing a greenfield site on e-health establishing a network for interlinking medical colleges across the country with the purpose of improving access to e-education. Disease surveillance and study is another attempt to blend all the available public health data and streamline access.
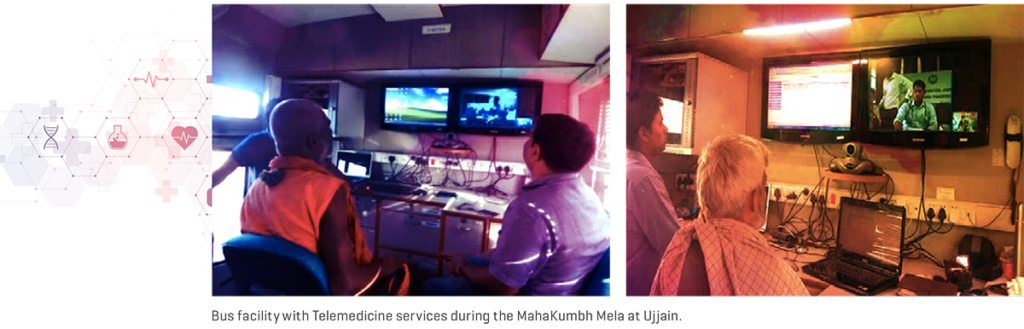
In India, during the MahaKumbh Melas festival, when large populations gather for religious prayers, the possibility of disease and infection increase substantially. The Government of Uttar Pradesh has utilized Telemedicine for provision of on-site medical care during this festival. There is a clear interest in providing remote care utilizing the latest technological advances in Telemedicine, not only in the public sector, but also in the private sector. Major players like Narayana Hrudayalaya, Apollo Telemedicine Enterprises, Asia Heart Foundation, Escorts Heart Institute, Amrita Institute of Medical Sciences, and Aravind Eye Care, are functioning virtually with appropriate support and updated technology from the Government and ISRO.
In response to the current COVID-19 crisis, the Indian Government has released a set of newly developed applications that use instant messaging platforms, such as WhatsApp, to enable a suite of virtual health-care services, including public messaging about behavioral modifications, epidemiological tracing, and access to virtual healthcare providers. Implementation of international Telemedicine projects led by the Ministry of External Affairs has strategically placed Indian Virtual Care on the global map.
Transmission of data safely, accurately, and effectively is another important consideration in healthcare, and even more so as Virtual Care practices expand across India. To that end, MoH&FW has developed a set of EHR (Electronic Health Record) standards in 2013, revised again in 2016. India seems to be on a digital transformation mission with its National Health Portal — a gateway to trusted health information including provider locations, ambulance services, blood banks, emergency helplines and general healthy living tips and guidance.

The Collaborative Digital Diagnosis System (CollabDDS) has been created with the intention to provide an integrated online environment to visualize medical and dental images for diagnosis and treatment planning. Remote Health Centers are connected to expert radiologists and doctors in Centers of Excellence, using appropriate tools and channels for data transmission and diagnostics. CollabDDS also provides specialists with a common platform for collaboration.
Thirteen thousand feet above sea level in the Himalayan Mountains, Apollo Hospitals has set up one of the highest Telemedicine stations in the world. This government-assisted initiative, known as the Himachal Pradesh Telehealth Services Project, aims to make quality healthcare more accessible to the people of this remote and hard-to-access region of northern India. The project has set up two Telemedicine stations — one at the community health center in the tiny village of Kaza, and another at the regional hospital in the mountain town of Keylong. Using dedicated satellite connections of 512 kbps, these locations are connected with Apollo specialists in various hospitals throughout the country using videoconferencing software.
Despite the prevalent use of modern medicine, there are many people in India who still believe in the traditional methods of medication, using herbal and home-based remedies, Ayurveda or natural medications. Ayush Telemedicine Network, promoted by State Health Society, Bihar, is a network of Telemedicine centers acting as next-generation delivery points for Ayush treatment (traditional, natural medicine) at District and Public Health Centers. Ensuring access to good quality healthcare at their doorstep, these centers are helping to minimize the gap in the health sector in Bihar and seek to promote the benefits of integrative, natural approaches to medicine to a wider audience.
Creative solutions to deliver healthcare to underserved parts of India are driving Telemedicine forward.
CARE ON WHEELS
With empathy comes interest, with interest comes creativity, and creativity fosters ideas — and some of these ideas convert into amazing initiatives that manifest themselves in real life and become commonplace. India has been gripped by a similar phenomenon that has attracted several world leaders who have come together to collaborate.
Sky Health Centers in collaboration with World Health Partners and the Melinda Gates Foundation, created a Mobile Telemedicine Bus for rural healthcare and medicine delivery. Children in rural Bihar do not receive adequate treatment, even though treatment for common illnesses like diarrhea is well known, inexpensive and widely available. The program seeks to train and enroll thousands of informal providers and create a massive network of franchisees to deliver more effective healthcare in rural areas of Bihar, an Indian state with more than 100 million residents.

Another notable initiative, ‘Swasthya Slate’ (which translates to “Health Tablet”) — is a ‘’lab in a rucksack” for off-the-grid village primary care. It is basically a mobile platform that allows you to conduct various kinds of diagnostics and pathology on a mobile phone or tablet. The kit consists of a digital thermometer, a blood pressure monitor, an easy-to-use heart rate sensor, an ECG system, a blood sugar monitor, and a water quality unit. It also has a solar panel to charge the unit. There are a variety of artificial intelligence-based apps for frontline health workers — not necessarily physicians, but trained providers. The Swasthya Slate has been deployed throughout rural parts of India.
AmbuPod (a patent-pending Telemedicine clinic and micro-ambulance on wheels), is another unique concept brought to life. It features an ambulance-cum-healthcare unit which is portable and can easily reach the remote areas of rural India. The main purpose of AmbuPod is to provide healthcare facilities to India’s rural population through Virtual Care. Not only does it carry medicinal and diagnostic supplies, it also has the ability to transport a patient and an attendant.
Asha Jyoti, a Women’s Healthcare Mobile Outreach Program, has been created to provide screening and referrals for breast cancer, cervical cancer, and osteoporosis. These services have already been provided to over 7,000 underserved patients over the past five years in Northern India, in the Punjab province and City of Chandigarh.

Tele-Eye Care Service, in Guntur Community Health Center was created in a Public Private Partnership (PPP) with Apollo Hospitals. Eye care is provided through digital medical equipment and telecommunications technology, even when a patient is located at a remote health center. This community outreach program using Telemedicine facilities has increased awareness of eye diseases, improved access to specialized healthcare, boosted local community empowerment, and provided employment opportunities. Early detection of sight-threatening disorders by Teleophthalmology and prompt treatment has helped decrease visual impairment considerably.
The Srikiran Institute of Ophthalmology connects satellite clinics with the main hospital to treat ophthalmology patients from different districts where specialized care is not available. Indian teleophthalmology projects like Sankara Nethralaya Teleophthalmology Project (SNTOP) and Aravind Teleophthalmology Network (ATN) have proven successful in the state of Tamilnadu, both in rural and secondary healthcare centers.
KNOWLEDGE + COMMUNICATION = POWER
Village Resource Centers (VRCs) provide satellite-based services and education programs in rural areas. They are one of the unique initiatives that use Satellite Communication (SATCOM) network and Earth Observation (EO) satellite data to reach out to the villages to address the needs of local people. ISRO has initiated this program with a view to integrate its capabilities in SATCOM and EO to disseminate a wide range of healthcare and education services to address the critical needs of rural communities.
- Telemedicine connects patients in villages to doctors located in cities and urban areas or superspecialty hospitals through a VSAT network.
- TeleEducation uses SATCOM to provide a virtual classroom to remote villages delivering education services to underserved populations.
- They offer career guidance and counseling to rural students and provide advisory support on issues related to agriculture, such as fertilization, pesticides, organic farming, crop insurance, and livestock and poultry management.
- They provide help in skills development, and deliver vocational training to rural populations.
- Other services include Panchayat planning, weather information, marketing information, watershed development, drinking water and e-Governance.
More than 6,500 programs have been implemented by the VRCs to date, addressing all these areas and more, such as awareness programs for female empowerment, supplementary education, computer literacy, micro credit, micro finance, and livelihood support. So far, more than 500,000 people have used the VRC services. There are around 500 VRCs which also connect to specialty hospitals and serve as providers to bring specialist services to the villages. Educating the masses is the only way to create learning, knowledge, and awareness, and lay the foundations for selfsufficiency. However, there remains a need to upscale the VRCs and link all the village Panchayats (village councils). This will help in efficient utilization of available resources in the villages, and also reduce migration from villages due to lack of basic health, education and information technology infrastructure.
Telemedicine today is one of the most vital SATCOM programs of ISRO. The Telemedicine Program is an innovative process combining the benefits of satellite communication and information technology with biomedical engineering and medical sciences to deliver much-needed healthcare services to remote and underserved regions of the country.
For northeastern states, a project known as ISRO-NEC (Indian Space Research Organization – North Eastern Council) joint Telemedicine project was formulated in July 2004, using satellite communication through VSAT to commission Telemedicine nodes in all the districts of the northeastern states including Sikkim. The major objective of the project is to connect the districtlevel hospitals to the specialty/super-specialty hospitals in the region and beyond for better healthcare at minimum cost using emerging technology. The major stakeholders of the project are ISRO, NEC and state governments of the region. NESAC (North Eastern Space Applications Center) is coordinating the installation and commissioning of the system, training, monitoring, and troubleshooting. So far, 25 Telemedicine Centers have been commissioned.
Another Virtual Care project known as Army Telemedicine Network for NER (North Eastern Region) has also been operational in the north-eastern states in collaboration with the Indian Army since March 2008. Under this network, a total of six Telemedicine centers have been commissioned in various army hospitals across the region. Under various different civilian networks, a further nine Telemedicine nodes were set up by ISRO in NER. These 40 Telemedicine centers are providing vital services to the people of NER in the health sector. Thousands of tele-consultancy and Continuing Medical Education programs (CME) have been carried out connecting many specialty and superspeciality hospitals like All India Institute of Medical Science, New Delhi; Narayana Hrudalaya, Bangalore; Amrita Institute of Medical Science, Cochin; Sri Ramachandra Medical College & Hospital, Chennai; Sanjay Gandhi PostGraduate Institute of Medical Science, Lucknow; Tata Memorial Centre, Mumbai; and Fortis Hospital, Noida. A large number of patients as well as clinicians are benefitting from this health service. NESAC is planning to revive the Telemedicine program in NER.

VIRTUAL CARE INITIATIVES IN URBAN INDIA
The AMTU (Amrita Mobile Telemedicine Unit) Is a fully air-conditioned bus featuring satellite-based video conferencing capability and is equipped with a wide range of medical devices including color echocardiography, cardiac treadmill, gastroscopy, colonoscopy, retinal camera, ultrasonography, X-ray radiography, electrocardiography, biochemical testing with a semi-auto analyzer, light microscopy and digital photography. The output from these devices can all be transmitted to a specialty hospital (typically Amrita) for review and expert opinion. It can connect to any healthcare center that has a Telemedicine facility. It is also equipped with the Amrita Health Information System (AHIS) Telemedicine Suite for electronically storing and transmitting patient data including medical images. The AMTU allows a wide range of healthcare services to be delivered with minimal expertise and infrastructure at the peripheral end. It also ensures increased utilization of medical facilities, manpower and technology while minimizing maintenance costs, effectively avoiding the need for fixed infrastructure and equipment. From the patient’s perspective, they can benefit from easier access to advanced healthcare and specialty consultations, saving considerable time and travel expenses.
The YOLO (You Only Live Once) kiosk and Health4U portable kiosk can screen people, capture health biometrics, and conduct basic diagnostic tests, all without a “human touch.” This includes measuring blood pressure, blood glucose, ECG, haemoglobin, lipid profile, BMI, fat, muscle, body temperature and oxygen saturation. The machine can even screen for common communicable diseases such as typhoid, malaria and dengue, and lets you videoconference with a doctor. They are being placed strategically in various easily accessible locations.
Another virtual and mobile initiative is the Arogyasree by ICMR (Indian Council of Medical Research), that is designing an ECG jacket for constant patient monitoring without the need for hospitalization.
Narayana Health (NH, formerly known as Narayana Hriduyalaya), a multi-speciality tertiary-level healthcare provider, is delivering affordable specialty health services remotely using Cisco’s Virtual Expertise Digital Solution, which can connect patients with NH specialists conveniently and efficiently, regardless of distance. The solution brings voice, video, and data to wherever patients are located and demonstrates how Telehealth and sensors within medical devices can create new opportunities for innovation. It also enables real-time telemetry of medical device data, audio, high-definition two-way video, ECG, other vitals and radiology, analytics of medical records and a web-based portal which supports mobile endpoints.
Dr Suresh Bada Math, Head of Telemedicine Centre and Forensic Psychiatry Services at the National Institute of Mental Health and Neuro Sciences (NIMHANS), said that a Telepsychiatry consultation is no less effective than in-person sessions. “There is a very large number of patients who need follow-up consultations and will benefit greatly from Teleconsultation. Each doctor will have around 30-40% of patients from remote locations for follow-ups and medication refills.” he said. Teleconsultation has, to some extent, helped bridge the distance, but the jury is still out on its efficacy.

LOOKING AHEAD
Despite the wide variety of Telehealth and Telemedicine initiatives in various regions of the country by both the government and private sector organizations, there is much work yet to be done in the field of Virtual Care. Technological improvisations have created some innovative solutions to everyday healthcare problems affecting the country, but we are still scratching the surface of what is possible compared to some digital health advances in the West.
For example, diabetes care is generally not available, accessible, or affordable to people living in rural parts of India. The Chunampet Rural Diabetes Prevention Project (CRDPP) is one noted exception and has been conceived with the aim of implementing comprehensive diabetes screening, prevention, and treatment using a combination of Telemedicine and personalized care in rural India. This project has been undertaken in a cluster of 42 villages in and around the Chunampet village in the state of Tamil Nadu in southern India. A Telemedicine van is being used to screen for diabetes and its complications using retinal photography, Doppler imaging, biothesiometry, and electrocardiography using standardized techniques. A rural diabetes center has also been set up to provide basic diabetes care to local residents.
Recent technological advances in India — such as the proliferation of fiber optic cables, the expanding bandwidth, and the licensing of private Internet service providers — has encouraged ISRO to set up an exclusive satellite, called HealthSAT, to bring Virtual Care to rural locations on a larger scale. The proposed satellite would not only serve remote areas of India but also those in other developing countries in Asia and Africa. There are 650 district hospitals, 3,000 taluk (subdistrict) hospitals, and more than 23,000 primary health centers in the country. ISRO aims to connect all of these in three phases — first, connecting the district hospital to specialty hospitals in major cities; second, the taluk-level hospitals; and finally, the primary health centers; so that no one, irrespective of their location, is deprived of a potentially lifesaving specialty consultation. As the network grows, private hospitals may be included as well. Although the network will initially be used for teleconsultation and postoperative consultation, in the future it may accommodate Telesurgery and Telerobotics. Theoretically, it is far easier to set up a robust telecommunication infrastructure in suburban and rural India than to place hundreds of medical specialists in these locations. India has realized that the future of telecommunications lies in satellite-based technology and fiber optic cables.
Virtual Care has helped save countless lives in crowded pilgrimage centers and military outposts connected with mobile Telemedicine units. For example, the Amrita Telemedicine Program reports that on January 13, 2003, the program’s first remote telesurgery procedure was performed. The Amrita Emergency Care Unit at Pampa was able to save the life of a pilgrim, thanks to a Telesurgical procedure using the local Telemedicine facility. The cardiothoracic surgeon guided the procedure remotely, and the pediatric cardiologist at Pampa performed the procedure. Mobile Telemedicine units were also rushed to the coasts and islands of India after the 2004 Tsunami to provide medical consultation and relief to victims of this devastating natural disaster.

Dr. Devi Shetty, a cardiac surgeon and the Chairman of Narayana Hrudayalaya, a hospital that has served thousands of patients through Virtual Care, said, “We have treated 17,400 patients using Telemedicine connectivity in various parts of India, mainly from rural India, and [a] few patients from outside India. We use both satellites as well as ISDN connectivity. Now, with ISRO, which is our associate in this project giving us the satellite connection for free, we have a [larger] game plan to offer healthcare [access] to African and other Asian countries.”
Impact India Foundations’s (IIF) Lifeline Express Hospital Train is another unique accomplishment, comprising a fully-equipped operating theatre, diagnostic center and postoperative ward, teaching facilities, laboratory and workshop. Using the vast rail network, it is shunted into rural sidings for a few weeks at a time, where it has become the nucleus of a comprehensive attack on causes of disability, involving the whole community. Effective, on-the-spot treatment is offered free of charge, together with health education and immunization, benefiting thousands of people each year. The original Lifeline Express, which had travelled the rail network since 1991, had to be decommissioned due to wear and tear, and five brand new carriages gifted by the Indian Ministry of Railways were renovated and equipped enabling this special train to be re-launched in August 2007.
With the help of HealthSAT, India’s Virtual Care initiative has the potential to provide specialized healthcare to millions of residents, especially in rural areas. This potential was summed up by Dr. Devi Shetty: “In terms of disease management, there is [a] 99% possibility that the person who is unwell does not require [an] operation. If you don’t operate you don’t need to touch the patient. And if you don’t need to touch the patient, you don’t need to be there. You can be anywhere, since the decision on healthcare management is based on history and interpretation of images and chemistry … so technically speaking, 99% of healthcare problems can be managed by doctors remotely — linked by Telemedicine.”
Although initially considered “futuristic” and “experimental”, Virtual Care is today a reality and is here to stay in India. Telemedicine has a variety of applications from patient care, education, and research, to medical administration and public health. People living in rural and remote areas struggle to access timely, good-quality, specialty medical care as specialist physicians tend to be located in urban areas. Virtual Care has the potential to bridge this distance and facilitate access to specialty care in these remote areas.
As part of Prime Minister Narendra Modi’s mission to create a Digital India, CSC (Common Service Center Scheme) and PMGDISHA (Pradhan Mantri Gramin Digital Saksharta Abhiyan) have come together to launch DigiGaon. DigiGaon aims to provide Virtual Care, education and skills training to ensure access to high quality, affordable healthcare for rural citizens. PMGDISHA has been extended to 60 million rural households to meet the goals of DigiGaon. The effective digitization of rural India will be key to the success of the Digital India mission and the DigiGaon initiative.
The leading cancer centers in India including National Cancer Grid, Tata Memorial Center and Navya, have come together to improve the delivery of cancer care by utilizing evidence-based treatment decisions. NRC (National Resource Center) at SGPGIMS, Lucknow has predominantly incorporated Telemedicine in their efforts to provide professional healthcare education remotely.
A National Medical College Network has also been set up by NRC and RRC (Regional Resource Center) to connect medical colleges, hospitals and remote areas together.
Continuing along the lines of education and the PAN India movement, live robotic surgery for tumor removal was recently transmitted from South Korea. Doctors connected from different parts of the country in real time and could interact through the telehealth platform. Many medical colleges have joined this bandwagon to extend knowledge beyond borders.
As with private startup innovations like Swasthya Slate, Health4U portable kiosk, and the YOLO kiosk, there are many other startups aspiring to deliver digital health. Portea is one notable startup that is working to provide healing at home. Portea arranges doctors, nurses, and physiotherapists for home visits who have cleared rigorous hiring standards and have had their backgrounds and medical knowledge verified by senior doctors. Portea also facilitates lab tests at home and medical equipment rentals, making healthcare more accessible and convenient for patients. Another prominent name among new startups is 1mg, which is serving as a one-stop online retail store for pharmacy and healthcare services. It provides access to medicines, supplements, skincare, and healthcare devices for diabetes and blood pressure, as well as access to healthcare services, lab tests, and ayurvedic treatments. There are numerous innovations and initiatives like this currently underway with the intention to not only provide easier access to healthcare for all, but also achieve significant gains in India’s Virtual Care and health tech industries.
BARRIERS TO GROWTH
The Virtual Care revolution in India has not been free of challenges and controversies. Of course, there are inevitable difficulties associated with the introduction of new systems and technologies. Healthcare providers fear loss of jobs and their practices through greater automation. Although the systems are user-friendly, there is the fear of the unknown in handling new technology and devices. Doctors have yet to become fully convinced and familiar with Telemedicine. There is also a lack of confidence among patients about the outcome and patient privacy. As with anything new, this sort of resistance is to be expected, and can only be improved through education. There is also a feeling that the initial investment is high and hence Telemedicine is financially not viable for many. In addition, there may be technical hitches that are frustrating and sometimes time consuming, such as low bandwidth, poor connectivity, and lack of interoperability standards for software. Health data privacy and conservative regulatory bodies who favor the status quo are other challenges to overcome.

Discussing HealthSAT, Dr. D. Lavanian, an Indian expert in Virtual Care affiliated with the Apollo Telemedicine Networking Foundation in Hyderabad, said: “[HealthSAT] is excellent, but some questions remain. Presently HealthSAT connectivity is expected to be given free of charge to certain government entities. This is unsatisfactory as a large proportion of healthcare in India is delivered by private entities.” Dr. Lavanian added: “On my request to ISRO to open this up to the private health sector, for a fee, I have not received any positive answer. This means that a large percentage of the population of India will [still] be denied healthcare via Telemedicine.”
Such challenges can invariably be overcome. In the late 1980s, when computers were first introduced to India, similar problems were experienced in different parts of the country. That is, people exhibited technophobia and expressed fears that computers would cause widespread job losses and would also be cost prohibitive. But the country overcame these challenges and fears, and eventually grew to become a superpower in the field of information technology. When it comes to the digital transformation of healthcare, India will no doubt rise to the occasion again.
CONCLUSION
Telemedicine is a promising tool for healthcare delivery and has been addressed by the Government of India since the turn of the century. The results have been very promising. Telemedicine cannot be the answer to all of India’s health problems, but it can be an important tool in addressing barriers to access and other health inequities. Services like Telehealth, Tele-education and Tele-home healthcare are proving to be indispensable. The importance of satellite communications is emphasized in the field of disaster management, when all terrestrial modes of communication are disrupted. International Telemedicine initiatives are bringing the world closer and distance is no longer a barrier in attaining quality healthcare.
Despite having so much potential, however, Telemedicine has not achieved the ‘boom’ in India that was widely anticipated. Lack of awareness and acceptance of new technology both by the public and professionals are holding it back. Back in 2015, the government had launched the Social Endeavour for Health and Telemedicine (SEHAT), a PAN-India health initiative to connect 60,000 healthcare organizations throughout the country and provide services to all irrespective of geographical location. Governments are now starting to take a keen interest in developing Virtual Care practices, resulting in a slow but steady increase in utilization in the public health domain. The current pandemic has definitely opened minds and accelerated implementation and widespread adoption. Hopefully in a few years, Telemedicine will have reached its full potential and become not just the common mode of access, but a way to remotely monitor, diagnose and treat patients in real time. The world of big data analytics and clinical decision support driven by machine learning is just around the corner. To paraphrase Neil Armstrong, Virtual Care is “One small step for IT, but one giant leap for Healthcare.”
Abbreviations
AHIS | Amrita Health Information System | ISRO | Indian Space Research Organisation |
AIIMS | All India Institute of Medical Sciences | IT | Information Technology |
AIMS | Amrita Institute of Medical Sciences | MoHFW | Ministry of Health and Family Welfare |
AMTU | Amrita Mobile Telemedicine Unit | NEC | North Eastern Council |
ATN | Aravind Teleophthalmology Network | NER | North Eastern Region |
BP | Blood Pressure | NESAC | North Eastern Space Applications Center |
CDAC | Centre for Development of Advanced Computing | NH | Narayana Health |
CHC | Community Health Centre | NIMHANS | National Institute of Mental Health And Neuro Sciences |
CME | Continuing Medical Education | NRC | National Resource Center |
CollabDDS | Collaborative Digital Diagnosis System | NRTN | National Rural Telemedicine Network |
CRDPP | Chunampet Rural Diabetes Prevention Project | ONCONET | Oncology Network |
CoVID-19 | CoronaVIrus Disease 2019 | SEHAT | Social Endeavour for Health and Telemedicine |
CSC | Common Service Centre | OOP | Out Of Pocket |
DIT | Department of Information Technology | PAN | Presence Across Nations |
ECG | Electrocardiogram | PC | Personal Computer |
EHR | Electronic Health Record | PPP | Public Private Partnership |
EO | Earth Observation | SATCOM | Satellite Communication |
RRC | Regional Resource Center | SEHAT | Social Endeavour for Health and Telemedicine |
GOI | Government Of India | SGPGIMS | Sanjay Gandhi Postgraduate Institute of Medical Sciences |
ICMR | Indian Council of Medical Research | SNTOP | Sankara Nethralaya Tele-Ophthalmology Project |
ICT | Information and Communication Technology | VRC | Village Resource Centre |
IIF | Impact India Foundation | VSAT | Very Small Aperture Terminal |
ISDN | Integrated Services Digital Network | YOLO | You Only Live Once |
References
Census of India – Government of India (2012). http://censusindia.gov.in/2011-prov-results/paper2/data_files/india/Rural_Urban_2011.pdf
Doctor’s Day: India faces critical shortage of doctors; Bihar worst affected. https://www.cnbctv18.com/market/data/doctors-day-india-faces-critical-shortage-of-doctors-bihar-worst-affected-3857551.htm
Telemedicine in India: Where do we stand? June 2019. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6618173/
Healthcare goes mobile: Evolution of teleconsultation and e-pharmacy in the new Normal. https://assets.ey.com/content/dam/ey-sites/ey-com/en_in/topics/health/2020/09/healthcare-goes-mobile-evolution-of-teleconsultation-and-e-pharmacy-in-new-normal.pdf
Outcome of 2 Case Studies on Field Telemedicine Application in Indian Setting. https://nmcn.in/pdf/Kumbh%20Mela%20Report.pdf
Telemedicine System – An Overview. https://www.sciencedirect.com/topics/engineering/telemedicine-system
Apollo Telemedicine Networking Foundation (ATNF). https://healthmarketinnovations.org/sites/default/files/Apollo%20Case%20Study.pdf
Village Resource Centre. https://www.isro.gov.in/applications/village-resource-centre
North Eastern Space Application Centre, Government of India. https://nesac.gov.in/village-resource-centre-vrc/
Evolving role of Telemedicine in Healthcare Delivery in India. https://www.iomcworld.org/open-access/evolving-role-of-telemedicine-in-health-care-delivery-in-india-2167-1079-1000260.pdf
Apollo Hospitals establishes Telemedicine in the Himalayas. https://vsee.com/blog/apollo-hospitals-establishes-telemedicine-stations-in-the-himalayas/
On-board the Lifeline Express, world’s first hospital train. April 16, 2018. https://www.rediff.com/news/report/pix-on-board-the-lifeline-express-worlds-first-hospital-train/20180416.htm
India’s Lifeline Express: World’s first hospital-train. The Economic Times. https://economictimes.indiatimes.com/infrastructure/indias-lifeline-express-worlds-first-hospital-train/offers-services-like-/slideshow/34768493.cms
Foreign Investment Promotion Board. The Economic Times. May 27, 2015. http://articles.economictimes.indiatimes.com/2015-05-27/news/62719540_1_fdi-inflows-fipb-foreign-investment-promotion-board
Asha Jyoti: Women’s Healthcare Mobile Outreach Program. https://www.clintonfoundation.org/clinton-global-initiative/asha-jyoti-womens-healthcare-mobile-outreach-program
Collaborative Digital Diagnosis System. https://collabdds.gov.in/
Ayushman Bihar. https://ayushmaanbihar.wordpress.com/
Ambupod: Future of Rural India. https://carbiketech.com/meet-ambupod-ambulance-rural-healthcare/
Lab in a rucksack – Washington Post – Nov 18, 2014. https://www.washingtonpost.com/news/innovations/wp/2014/11/18/this-indian-start-up-could-disrupt-health-care-with-its-powerful-and-affordable-diagnostic-machine/
Path lab in a tablet. https://www.downtoearth.org.in/news/path-lab-in-a-tablet-37975
Swasthya Slate – TheBetterIndia.com https://www.thebetterindia.com/49931/swasthya-slate-kanav-kahol-delhi-diagnostic-tests/
Telemedicine @ National Resource Center & Mobile Telemedicine Van. https://nmcn.in/pdf/1%20Dr.S.K.Mishra%20SGPGI%20Telemedicine%20Programme.pdf
YOLO ATMs can revolutionize Primary Healthcare. https://homegrown.co.in/article/800701/how-yolo-health-atms-can-revolutionise-primary-health-care-in-india
Telemedicine in Rural India. https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0030082
Hospital on Wheels – Amrita starts free Medical Camps. https://amritaworld.org/healthcare/hospitals/satellite-hospitals/amritakripa-hospital-mysuru/hospital-on-wheels-amrita-to-start-free-medical-camps-with-solar-powered-telemedicine-van/
Narayana Health – Advances in Telemedicine and virtual diagnostics. https://www.ciol.com/narayana-health-advances-on-telemedicine-and-virtual-diagnostics/
Narayana Health website: https://www.narayanahealth.org/csr-health
Mental health experts switchto tele-consultation mode. Indiatimes. https://health.economictimes.indiatimes.com/news/diagnostics/mental-health-experts-switch-to-teleconsultation-mode/76146808
Telemedicine in the Himalayas: Operational Challenges – A Preliminary Report Telemedicine and e-Health. May 2016, ahead of print. doi:10.1089/tmj.2015.0249. http://caho.in/?p=3754
Teleophthalmology-based rural eye care in India. Telemed J E Health 2007. Jun;13(3):313-21. doi: 10.1089/tmj.2006.0048. https://pubmed.ncbi.nlm.nih.gov/17603834/
Sankara Nethralaya Mobile Teleophthalmology Camp https://www.supportsankaranethralaya.org/tele_mobile_tele_ophthalmology.html
Development of TeleMedicine in India – Results and Future. https://nmcn.in/nrc/ppt/Telemedicine%20for%20Rural%20Masses%20current%20initiative%20and%20future%20scope%20Oditelecon.pdf
Portea Heal at Home. https://www.portea.com/
1mg Online Pharmacy. https://www.1mg.com/
Healthcare goes mobile. Evolution of teleconsultation and e-pharmacy in the new normal. https://assets.ey.com/content/dam/ey-sites/ey-com/en_in/topics/health/2020/09/healthcare-goes-mobile-evolution-of-teleconsultation-and-e-pharmacy-in-new-normal.pdf
Additional resources for Telemedicine in India: www.telemedicineindia.com

